Macra Quality Measures

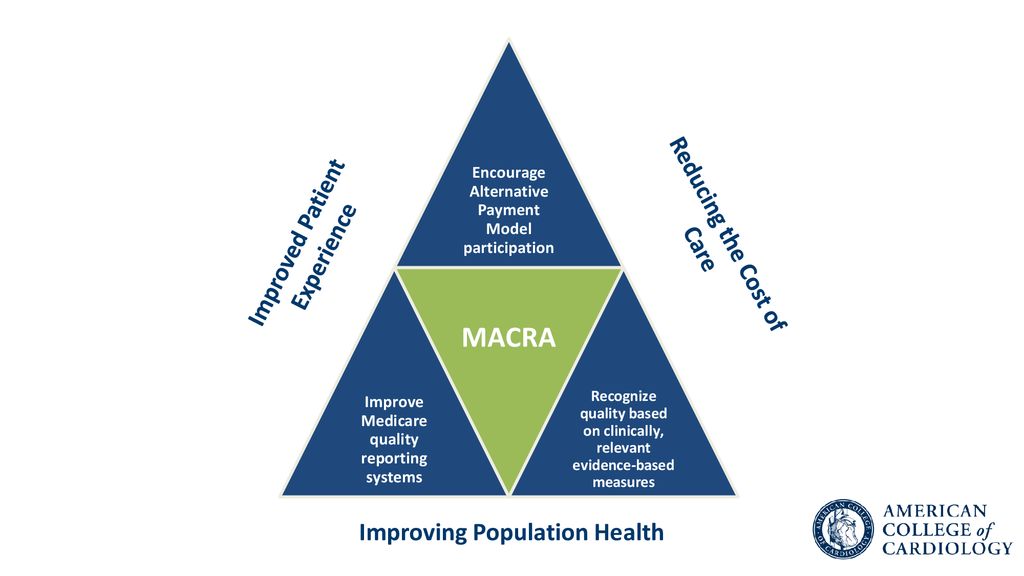
Macra builds on work pioneered by ncqa for almost 30 years.
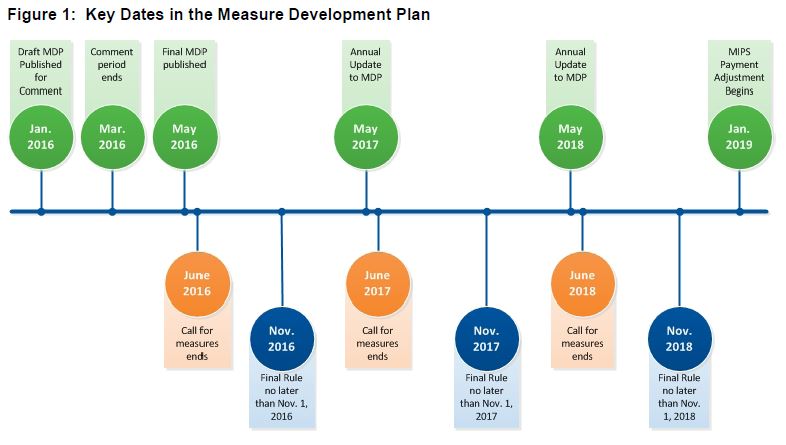
Macra quality measures. These measures come in 2 flavors. 2020 quality measure development plan annual report zip june 25 2020. Types of macra quality measures. Commenters informed the creation of this final cms quality measure development plan mdp.
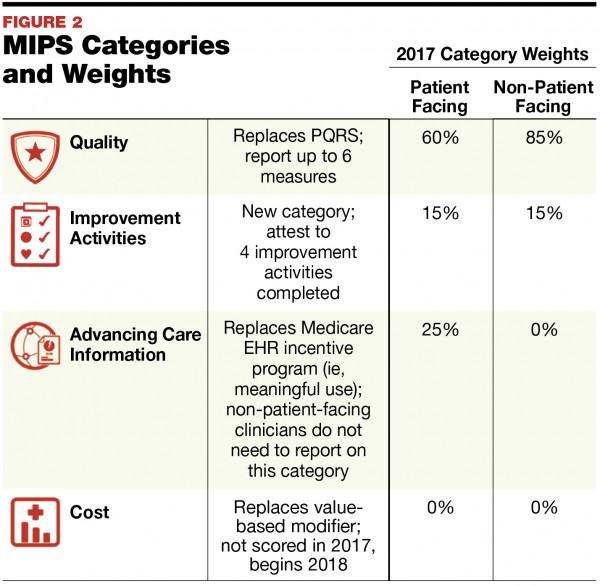
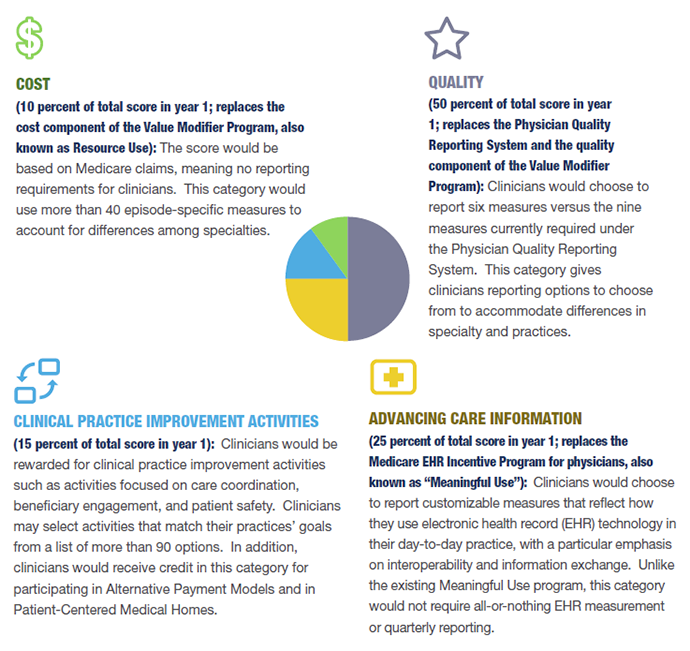
For hospitalists the quality category will be 70 of their mips score in 2019. They have some very important. Developing measures for the quality payment program. Macra provides both a mandate and an opportunity for cms to leverage quality measure development as a key driver to further the aims of the cms quality strategy.
Most hospitalists will not have enough quality measures to report and will be subject to a validation process to ensure there were no other measures available to them. Ncqa programs included in macra. The macra patient relationship codes are healthcare common procedure coding system hcpcs level ii modifier codes that enable clinicians to self identify their relationship with and responsibility for a patient at the time of furnishing an item or service. Abg qcdr shared qcdr and mips measures defined.
To meet these requirements cms contracted with the american academy of hospice and palliative medicine aahpm to develop two patient reported outcome performance measures pro pms in the areas of pain. Qcdr measures or mips measures. Implementing the cms quality measure development plan. They have some very important.
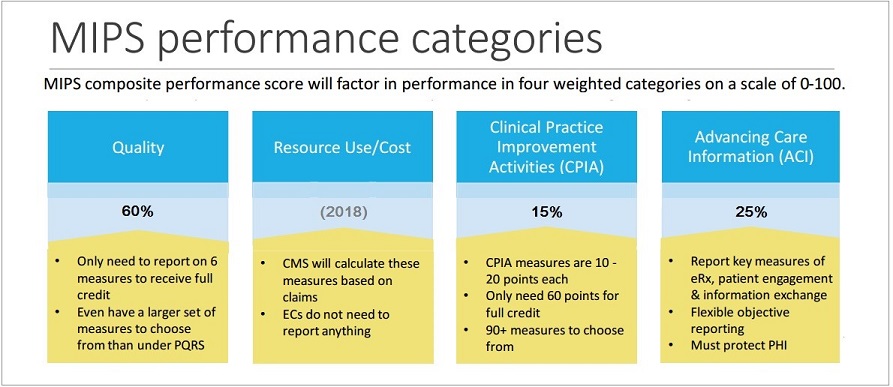
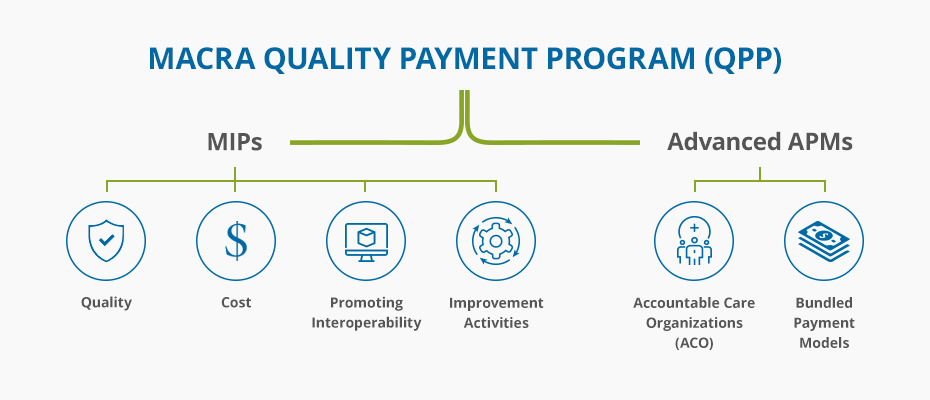
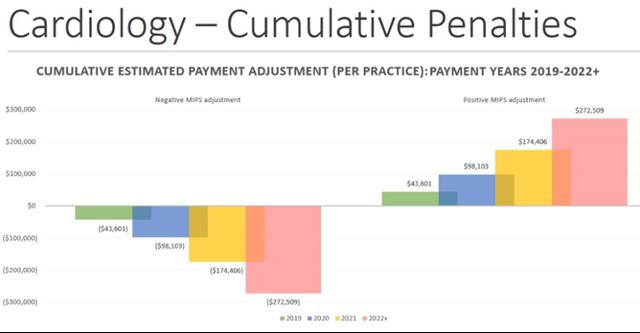
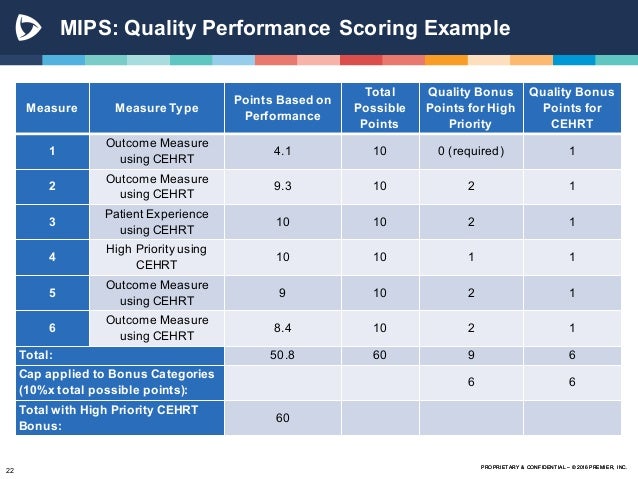
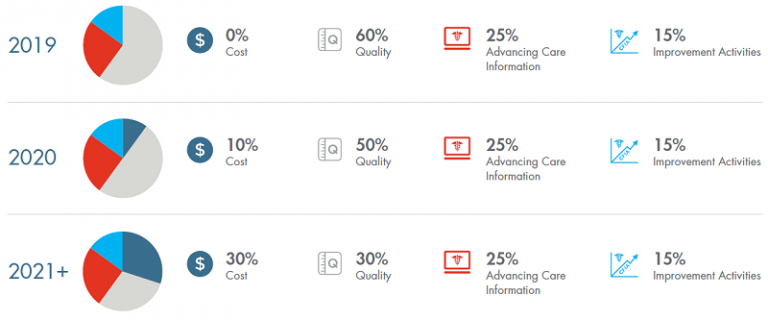
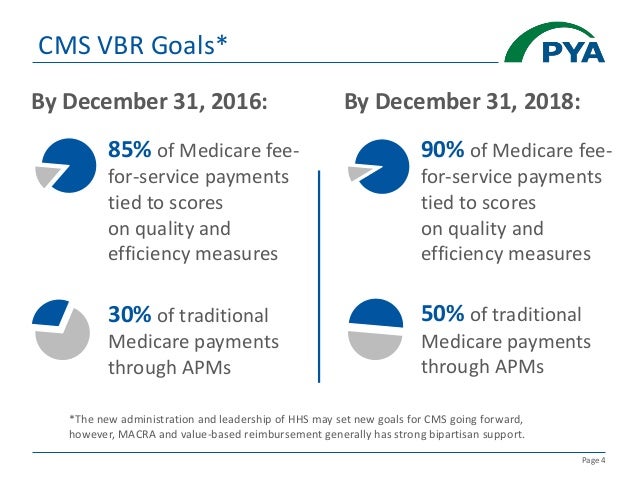
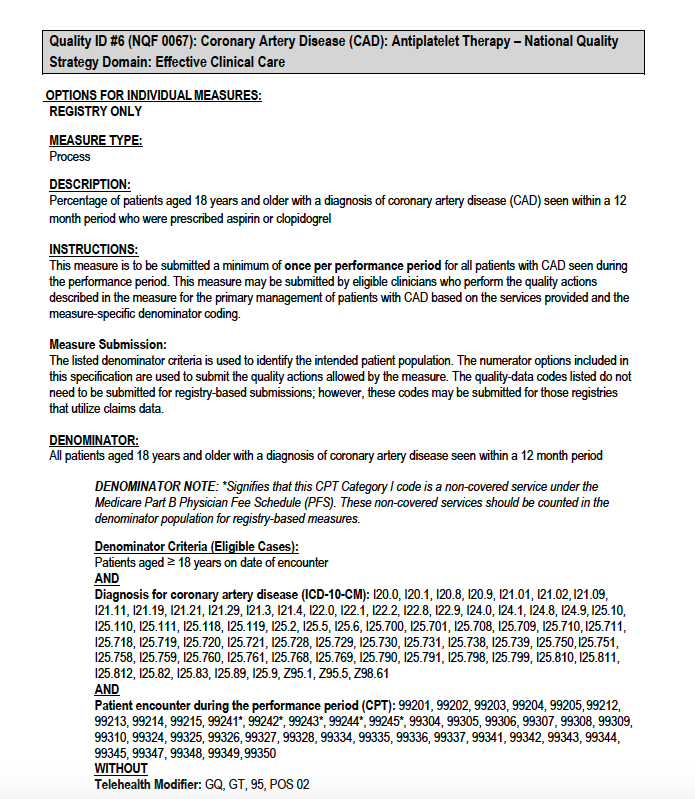
Quality measures account for 75 of your composite performance score cps and you can only report a maximum of 6 measures. Under the medicare access and chip reauthorization act of 2015 macra the centers for medicare and medicaid services cms was directed to develop performance measures for clinicians. Read shm s macra and the quality payment program frequently asked questions faqs for further. Medicare access and chip reauthorization act of 2015 macra funding opportunity.
2018 macra quality measures. Types of macra quality measures. Abg qcdr shared qcdr and mips measures defined. Measure development for the quality payment program cooperative agreement awardees on september 21 2018 we selected 7 applicants to receive cooperative agreement awards through the medicare access and chip reauthorization act of 2015 macra funding.
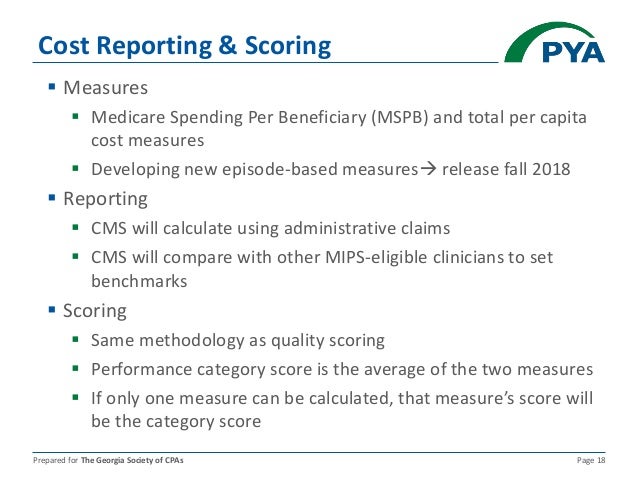
These measures come in 2 flavors. Qcdr measures or mips measures. Macra requires the plan to be posted on the cms gov website by may 1 2016. Measure development plan mdp annual reports meet macra s requirement to report our progress every year in.